Hemorrhoidectomy recovery follows a predictable yet intensely challenging pattern, with the most difficult period typically occurring between days three to five post-surgery. Understanding what constitutes the worst day after this procedure can help patients prepare mentally and physically for the recovery journey ahead. While individual experiences vary considerably, the peak discomfort period represents a critical phase where pain levels reach their zenith, accompanied by various physical and emotional challenges that require careful management and realistic expectations.
The concept of a “worst day” encompasses multiple factors beyond simple pain measurement. Patients often experience a convergence of symptoms including severe anal discomfort, difficulty with bowel movements, sleep disruption, and the psychological impact of prolonged recovery. The severity of symptoms during this period often surprises patients , particularly those who may have underestimated the intensity of post-operative discomfort despite thorough pre-surgical counselling.
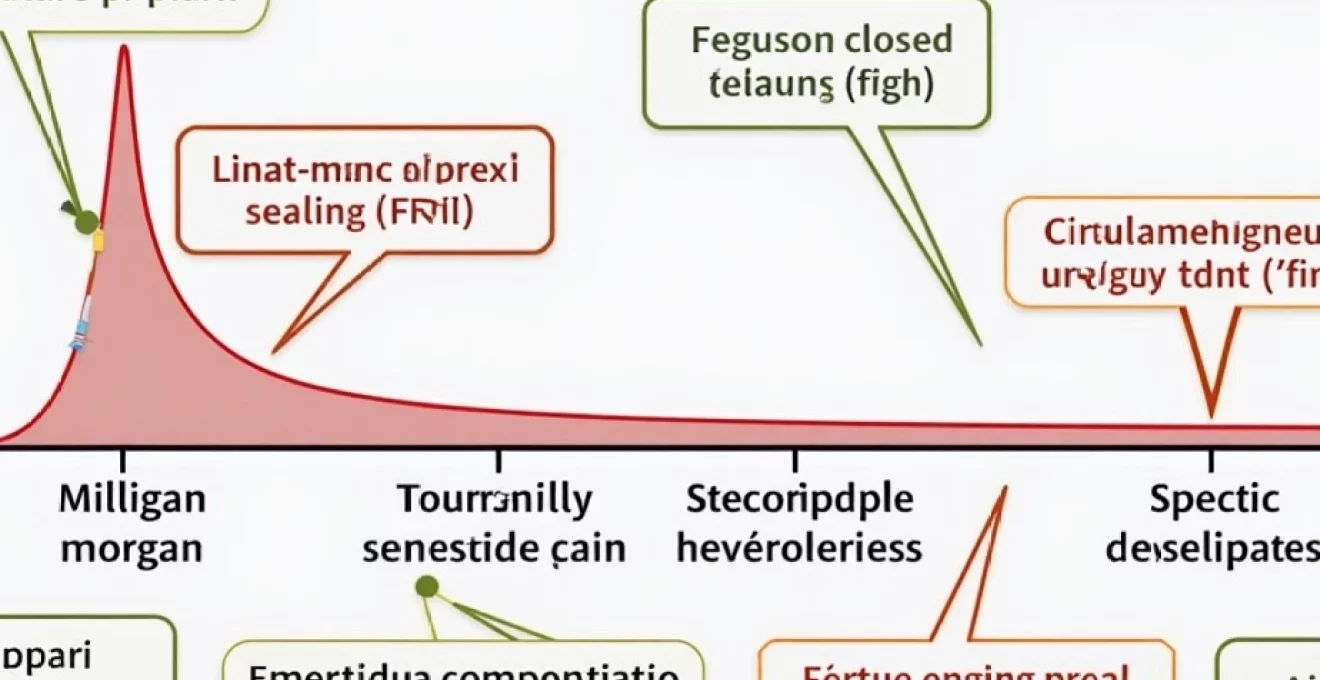
Peak pain timeline: understanding day 3-5 Post-Hemorrhoidectomy recovery
The post-hemorrhoidectomy pain trajectory follows a distinct pattern that healthcare professionals have observed consistently across different patient populations. Initial post-operative pain in the immediate 24-48 hours is typically managed effectively through residual anaesthetic effects and aggressive pharmaceutical intervention. However, the third to fifth day post-surgery represents the nadir of the recovery experience, when inflammatory responses peak and the body’s natural healing processes create maximum tissue tension and sensitivity.
During this critical period, pain scores on the visual analogue scale frequently reach 7-9 out of 10, with many patients describing the discomfort as more intense than the original hemorrhoidal symptoms that necessitated surgery. The pain is characteristically described as throbbing, burning, and sharp , often radiating beyond the immediate surgical site to affect the entire pelvic region. This intensification occurs as surgical oedema reaches its maximum, wound healing processes accelerate, and the protective effects of initial post-operative medications begin to diminish.
Milligan-morgan technique recovery patterns and pain intensity curves
The traditional open hemorrhoidectomy technique, known as the Milligan-Morgan method, creates specific pain patterns that patients should anticipate. This approach leaves wounds open to heal by secondary intention, resulting in prolonged exposure of sensitive perianal tissues. Patients typically experience their worst day around day four, when wound edges begin contracting and granulation tissue formation creates significant tension. The open nature of these wounds means that every bowel movement, sitting position change, and even walking can trigger severe discomfort.
Ferguson closed hemorrhoidectomy: specific Day-by-Day pain progression
The Ferguson technique involves primary closure of surgical wounds, creating a different pain timeline compared to open procedures. While initial pain may be less severe due to wound approximation, the worst day often occurs earlier, typically around day three, when suture tension peaks and tissue oedema reaches maximum levels. Patients frequently report a sensation of internal pressure and tightness that can be particularly distressing during defaecation attempts.
Ligasure vessel sealing system: Post-Operative pain management expectations
Modern electrothermal vessel sealing technology, such as the Ligasure system, has modified traditional pain patterns in hemorrhoidectomy recovery. The thermal tissue sealing creates different wound characteristics, often resulting in the worst day occurring around day three to four. The electrothermal energy promotes faster tissue healing but can initially create more intense inflammatory responses. Patients may experience burning sensations that persist beyond typical surgical pain, requiring specific management strategies.
Circular stapled hemorrhoidopexy (PPH): atypical pain patterns during worst recovery phase
The stapled hemorrhoidopexy procedure presents unique recovery challenges, with the worst day often manifesting differently from traditional excisional techniques. Pain typically peaks around day two to three, characterised by deep pelvic pressure and unusual sensations related to the circular staple line. Some patients report feeling as though they need to defaecate constantly , a sensation known as tenesmus, which can be particularly distressing during the worst recovery period.
Severe Post-Operative complications: recognising critical warning signs
While intense pain and discomfort are expected during the worst day of hemorrhoidectomy recovery, certain symptoms indicate serious complications requiring immediate medical intervention. Understanding the distinction between expected severe symptoms and pathological complications can be life-saving. Complications during the worst recovery period are particularly dangerous because normal post-operative pain can mask warning signs of serious problems.
The most concerning complications typically manifest when patients are already experiencing peak discomfort, making recognition challenging. Healthcare providers emphasise that any symptom that seems disproportionate to expected recovery patterns warrants immediate evaluation. The psychological impact of severe pain can also impair judgement, making it crucial for patients and caregivers to maintain vigilance for specific warning signs that transcend normal recovery discomfort.
Urinary retention following spinal anaesthesia: emergency intervention protocols
Urinary retention represents one of the most common serious complications during the worst recovery period, particularly following spinal or epidural anaesthesia. The inability to urinate for more than eight hours post-operatively, or the sensation of incomplete bladder emptying with severe discomfort, requires immediate catheterisation. This complication can transform an already difficult worst day into a medical emergency, as bladder overdistension can cause permanent damage to detrusor muscle function.
Secondary haemorrhage risk: identifying delayed bleeding between days 7-14
While the worst pain day typically occurs earlier in recovery, secondary haemorrhage risk peaks between days seven to fourteen when surgical sutures dissolve and scabs separate. Patients experiencing their worst day may not immediately recognise that fresh bleeding exceeding an egg cup volume within 24 hours constitutes a surgical emergency. The combination of severe pain and significant bleeding creates a particularly dangerous scenario requiring urgent colorectal surgical consultation.
Anal stenosis development: early recognition of stricture formation
Anal stenosis can begin developing during the worst recovery period, manifesting as progressive difficulty passing stool despite adequate softening measures. Early recognition involves identifying when defaecation becomes impossibly difficult rather than merely painful. The distinction is crucial because early intervention with gentle dilatation can prevent permanent stricture formation that would require additional surgical procedures.
Septic complications: perianal abscess and necrotising fasciitis indicators
Septic complications during the worst recovery day present with systemic symptoms including fever above 38.5°C, rapidly spreading erythema beyond the immediate surgical site, and malodorous discharge. Necrotising fasciitis, while rare, can develop rapidly and presents with disproportionate pain relative to visible signs, skin colour changes, and rapidly spreading infection markers. These complications require emergency surgical intervention and broad-spectrum antibiotic therapy.
Pharmaceutical pain management protocols for maximum discomfort days
Effective pain management during the worst recovery period requires a multimodal approach combining different medication classes to address various pain mechanisms. Traditional reliance on opioid medications alone proves inadequate for managing the complex pain syndrome associated with hemorrhoidectomy recovery. The most effective protocols incorporate scheduled administration of analgesics rather than as-needed dosing, preventing pain breakthrough that becomes exponentially more difficult to control once established.
The pharmacological challenge lies in balancing adequate pain control with the need to maintain bowel function and prevent medication-induced constipation, which can exacerbate surgical site pain. Modern pain management protocols emphasise pre-emptive analgesia , beginning before pain peaks and maintaining consistent therapeutic levels throughout the worst recovery period. This approach has significantly improved patient outcomes and reduced the psychological trauma associated with inadequate pain control during critical recovery phases.
Topical anaesthetic preparations, including lidocaine gels and suppositories, provide localised relief that complements systemic medications. These preparations can be particularly effective when applied before anticipated painful activities such as defaecation or sitting for extended periods. The combination of oral analgesics with topical preparations often provides superior pain control compared to either approach used independently, particularly during the worst recovery days when pain intensity peaks.
Anti-inflammatory medications play a crucial role in managing the inflammatory component of post-hemorrhoidectomy pain. Non-steroidal anti-inflammatory drugs, when not contraindicated, can significantly reduce tissue swelling and associated discomfort. However, careful consideration must be given to bleeding risks, particularly during the secondary haemorrhage risk period. The timing and selection of anti-inflammatory agents requires careful coordination with the surgical team to optimise benefits while minimising complications.
Physical symptoms and bodily functions during peak recovery distress
The worst day of hemorrhoidectomy recovery encompasses far more than isolated pain, affecting multiple bodily systems and functions in ways that compound the overall distress experience. Physical symptoms during this period create a cascade of complications that can transform routine activities into significant challenges. Understanding these interconnected symptoms helps patients and caregivers develop appropriate management strategies and maintain realistic expectations about the recovery timeline.
Systemic effects during the worst recovery period often include fatigue, nausea, and generalised malaise that extend beyond the immediate surgical site. The body’s inflammatory response to surgical trauma creates widespread effects that can impact appetite, sleep patterns, and overall energy levels. These systemic symptoms, while normal, can significantly impact a patient’s ability to cope with peak pain levels and may require specific interventions to prevent complications such as dehydration or nutritional deficiency.
Defaecation challenges: managing first bowel movement Post-Surgery
The first bowel movement following hemorrhoidectomy typically occurs during or shortly after the worst recovery period, creating a perfect storm of anxiety and physical discomfort. This milestone often represents the most feared aspect of recovery, with many patients experiencing severe anticipatory anxiety that can worsen pain perception. The combination of surgical site sensitivity, fear-induced muscle tension, and potential constipation from pain medications creates a complex challenge requiring careful preparation and support.
Successful navigation of this challenge requires coordinated preparation including adequate stool softening, optimal pain medication timing, and psychological support. Many patients find that the anticipation proves worse than the actual experience , particularly when appropriate preparatory measures have been implemented. Positioning strategies, breathing techniques, and relaxation methods can significantly improve the experience and reduce associated trauma.
Perianal oedema and tissue swelling: expected inflammation patterns
Tissue swelling reaches maximum levels during the worst recovery period, creating significant discomfort beyond the immediate surgical wounds. Perianal oedema can extend several centimetres beyond the surgical site, affecting sitting tolerance, walking comfort, and general mobility. The swelling often creates a sensation of fullness and pressure that patients describe as feeling like they are sitting on a tennis ball or similar object.
Management of oedema during this critical period involves elevation strategies, cold therapy application, and gentle compression techniques. The inflammatory response is necessary for healing but can be moderated through appropriate interventions without compromising recovery outcomes. Understanding that swelling will gradually resolve helps patients maintain perspective during the most challenging recovery days.
Sleep disruption patterns: positioning strategies for nocturnal comfort
Sleep disturbance during the worst recovery period creates additional challenges by reducing pain tolerance and impairing the body’s natural healing processes. Finding comfortable sleeping positions becomes increasingly difficult as pain intensifies and swelling peaks. Traditional sleeping positions may become impossible, requiring creative adaptations and positioning aids to achieve adequate rest.
Effective sleep strategies during this period include elevated positioning, side-lying techniques, and the use of specialised cushions or supports. Sleep fragmentation is almost universal during the worst recovery period, but implementing consistent sleep hygiene practices and pain medication timing can improve overall rest quality. The relationship between adequate sleep and pain perception creates a critical cycle that requires active management to prevent deterioration.
Nutritional interventions and dietary modifications for optimal healing
Nutritional status during the worst recovery period significantly impacts healing outcomes and pain management effectiveness. The challenge lies in maintaining adequate nutrition when appetite is often diminished due to pain and medications, while simultaneously ensuring bowel function remains optimal to prevent constipation-related complications. Strategic dietary planning becomes crucial during this period to support healing while minimising gastrointestinal distress that could exacerbate surgical site pain.
Protein requirements increase significantly during the worst recovery period as the body repairs surgical wounds and manages inflammatory responses. However, traditional high-protein foods may be difficult to consume due to pain medication side effects or general malaise. Creative approaches to protein intake become necessary, including liquid supplements, smoothies, and easily digestible options that provide essential amino acids for tissue repair without creating additional digestive stress.
Hydration assumes critical importance during peak recovery distress, as dehydration can worsen constipation, intensify pain perception, and impair healing processes. The challenge involves consuming adequate fluids when mobility is limited and bathroom visits are painful. Strategic fluid intake timing, including increased consumption between meals and careful coordination with medication schedules, helps maintain optimal hydration status throughout the worst recovery period.
Fibre intake requires careful balancing during this critical period. While adequate fibre prevents constipation that could worsen surgical site pain, excessive fibre during the worst recovery period may create gas production and bowel distension that increases discomfort. Soluble fibre sources often prove more tolerable than insoluble varieties during peak pain periods, providing stool-softening benefits without excessive bulk that might stress healing tissues during defaecation.
When to contact your colorectal surgeon: emergency thresholds and red flags
Distinguishing between expected severe symptoms during the worst recovery period and complications requiring immediate medical intervention can be challenging but potentially life-saving. The intensity of normal post-hemorrhoidectomy pain can mask warning signs of serious complications, making it crucial for patients and caregivers to understand specific thresholds that warrant emergency contact with the surgical team.
Temperature elevation above 38.5°C represents a clear threshold requiring immediate surgical consultation, particularly when accompanied by increasing pain or unusual discharge. While low-grade fever can be normal during the inflammatory phase of healing, significant temperature elevation suggests possible infection requiring urgent intervention. The combination of fever with rapidly worsening pain creates a particularly concerning scenario that should never be dismissed as normal recovery progression.
Bleeding thresholds during the worst recovery period require careful assessment, as some bleeding is expected but excessive haemorrhage constitutes a surgical emergency. Any bleeding that exceeds one egg cup volume within 24 hours, or continuous bleeding that fails to respond to direct pressure and positioning, requires immediate evaluation. The distinction between normal healing discharge and pathological bleeding becomes crucial during this period when patients may attribute concerning symptoms to expected recovery challenges.
Inability to urinate for more than eight hours, or severe difficulty with urination accompanied by bladder distension, represents an absolute indication for emergency consultation. This complication can develop rapidly during the worst recovery period, particularly in male patients or those who received spinal anaesthesia. Prompt recognition and treatment of urinary retention prevents permanent bladder damage and can transform the recovery experience from unbearable to manageable.
Psychological distress indicators, while often overlooked, can signal the need for additional support during the worst recovery period. Persistent inability to cope with pain despite appropriate medication, expressions of self-harm, or complete loss of confidence in recovery progress may require enhanced support services. The emotional toll of severe post-operative pain should not be underestimated, and comprehensive care includes addressing psychological as well as physical aspects of recovery during the most challenging periods.