Accidental hairspray exposure to the eyes is a surprisingly common household emergency that affects thousands of people annually. The combination of alcohol-based solvents, polymer compounds, and pressurised propellants in modern hairspray formulations can cause immediate discomfort and potential ocular damage. Understanding the proper response protocols and chemical composition of these products is essential for both prevention and effective treatment. Most hairspray-related eye injuries are minor when handled correctly, but the pressurised nature of aerosol delivery systems and the specific chemical components require immediate and appropriate intervention to prevent complications.
Immediate eye irrigation protocols following hairspray contact
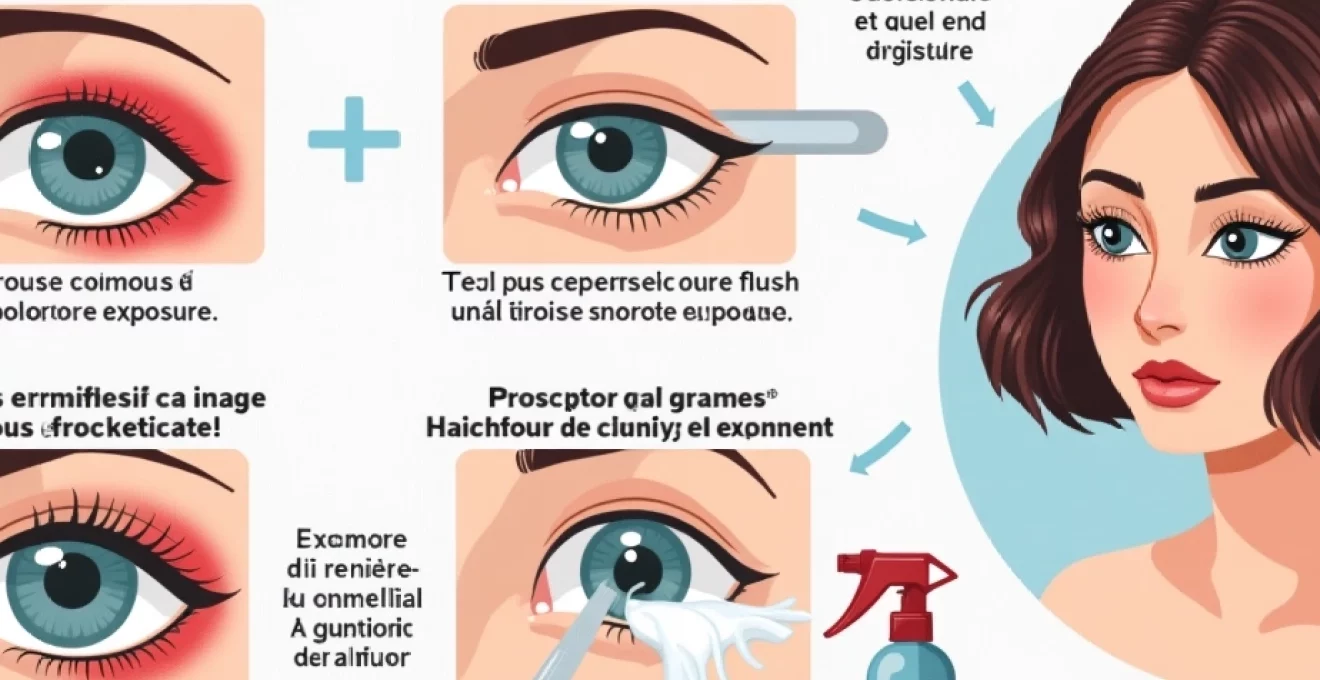
The moment hairspray contacts your eye, the priority is immediate dilution and removal of the chemical irritants. Time is critically important in minimising tissue damage and reducing the severity of symptoms. The standard protocol requires continuous irrigation for a minimum of 15-20 minutes, regardless of the apparent severity of the exposure. This duration ensures adequate dilution of alcohol-based solvents and removal of polymer residues that may adhere to the ocular surface.
Sterile saline solution flush technique for chemical eye exposure
Sterile saline solution represents the gold standard for ocular irrigation following hairspray exposure. The isotonic nature of saline prevents additional cellular damage that might occur with hypotonic or hypertonic solutions. When using saline, position the affected eye lower than the unaffected eye to prevent cross-contamination. Direct the saline stream from the inner corner of the eye outward, allowing gravity to assist in removing contaminants. Professional emergency responders recommend using at least 500ml of sterile saline for thorough irrigation of chemical exposures.
Tap water emergency irrigation when saline unavailable
When sterile saline is not immediately available, clean tap water provides an acceptable alternative for emergency irrigation. The temperature should be lukewarm to room temperature, as hot water can increase tissue damage and cold water may cause additional discomfort. Municipal water supplies contain chlorine and other chemicals, but the benefits of immediate irrigation far outweigh the minimal risks associated with these additives. Continue irrigation with tap water for the full 15-20 minute duration, maintaining a gentle but steady flow to avoid additional mechanical trauma to the eye.
Contact lens removal procedures during hairspray contamination
Contact lens wearers face additional complications during hairspray exposure, as polymer compounds and alcohol solvents can bind to lens materials. Remove contact lenses immediately if they move freely and can be extracted without force. However, if lenses appear stuck or cause additional pain during removal attempts, begin irrigation immediately and allow the flushing action to naturally loosen the lenses. Never attempt to force removal of contact lenses that resist gentle extraction, as this may cause corneal abrasions or push chemical irritants deeper into the eye tissues.
Eye position and flow direction for optimal chemical dilution
Proper positioning during irrigation maximises chemical removal whilst preventing contamination of the unaffected eye. Tilt your head to the side with the affected eye positioned lower, creating a natural drainage pathway. Hold the eyelids open with clean fingers, ensuring the irrigation solution contacts all areas of the conjunctiva and cornea. The flow should proceed from the nasal corner toward the temporal corner, following the natural curvature of the eye. This technique prevents hairspray residues from pooling in the conjunctival sacs and ensures thorough cleansing of both upper and lower eyelid surfaces.
Chemical composition analysis of common hairspray formulations
Modern hairspray products contain complex chemical formulations designed to provide hold whilst maintaining user safety under normal conditions. However, when these products contact sensitive ocular tissues, even “safe” ingredients can cause significant irritation and potential damage. Understanding the specific components helps predict the severity of exposure and guides appropriate treatment decisions. The concentration and combination of active ingredients vary significantly between manufacturers and product types, with professional-grade formulations typically containing higher concentrations of active polymers and solvents.
Ethyl alcohol and isopropyl alcohol ocular toxicity effects
Alcohol compounds serve as primary solvents in hairspray formulations, typically comprising 25-50% of the total product volume. Ethyl alcohol exposure causes immediate burning sensations and can lead to conjunctival inflammation and temporary corneal epithelial damage. Isopropyl alcohol presents greater toxicity concerns, as it penetrates ocular tissues more readily and can cause more severe inflammatory responses. Both alcohol types can disrupt the tear film’s natural protective barrier, leading to increased susceptibility to secondary infections. Prolonged exposure to these solvents may result in corneal clouding and potential vision changes requiring medical intervention.
Polyvinylpyrrolidone and vinyl acetate copolymer reactions
Polymer compounds provide the styling hold in hairspray formulations but can cause mechanical irritation when they contact ocular surfaces. Polyvinylpyrrolidone (PVP) forms film-like deposits that can adhere to the corneal surface, creating a foreign body sensation and potential visual disturbances. Vinyl acetate copolymers can trigger allergic reactions in sensitive individuals, manifesting as conjunctival redness, swelling, and excessive tearing. These polymer deposits require thorough irrigation to prevent formation of adherent films that may necessitate mechanical removal by healthcare professionals.
Propellant gas exposure from butane and isobutane compounds
Hydrocarbon propellants such as butane and isobutane create additional hazards beyond their role in product delivery. These compounds can cause rapid tissue cooling upon contact, potentially leading to frostbite-like injuries of the ocular surface. The pressurised nature of propellant delivery can also create mechanical trauma, particularly when the aerosol nozzle is positioned close to the eye during accidental discharge. High-velocity propellant streams may cause corneal abrasions or more serious penetrating injuries requiring immediate ophthalmological assessment.
Dimethyl ether and hydrofluorocarbon propellant hazards
Modern environmentally-friendly hairsprays often utilise dimethyl ether or hydrofluorocarbon propellants as alternatives to traditional hydrocarbon systems. Dimethyl ether exposure can cause significant conjunctival irritation and may lead to corneal epithelial defects in severe cases. Hydrofluorocarbon propellants, whilst generally less toxic than older chlorofluorocarbon systems, can still cause chemical burns when concentrated exposure occurs. These newer propellant systems may also contain additional stabilising compounds that can contribute to ocular toxicity and complicate treatment protocols.
Ocular surface damage assessment and symptom recognition
Recognising the signs and symptoms of hairspray-induced ocular injury is crucial for determining appropriate treatment pathways and identifying cases requiring professional medical intervention. The spectrum of potential injuries ranges from mild conjunctival irritation to severe chemical burns affecting multiple layers of ocular tissue. Initial symptoms may not accurately reflect the ultimate severity of injury, as some chemical reactions continue to progress after the initial exposure. Pain levels can vary significantly between individuals and do not reliably correlate with the extent of tissue damage.
Immediate symptoms typically include burning or stinging sensations, excessive tearing, and involuntary eyelid spasm (blepharospasm). Visual symptoms may include blurred vision, light sensitivity (photophobia), and the sensation of foreign material in the eye. Redness and swelling of the conjunctiva usually develop within minutes of exposure and may progress over several hours. More severe exposures can cause corneal cloudiness, visible white or gray areas on the corneal surface, and significant eyelid swelling that may prevent normal eye opening.
The delayed presentation of symptoms is particularly concerning with hairspray exposures, as polymer compounds may continue to release active ingredients over time. Some individuals may experience initial mild symptoms that worsen over 6-12 hours as chemical reactions progress. Vision changes, including decreased visual acuity, halos around lights, or complete vision loss in the affected eye, indicate serious injury requiring immediate emergency medical care. Persistent pain that worsens rather than improves with irrigation also suggests significant tissue damage requiring professional assessment.
Medical intervention thresholds and emergency response protocols
Determining when professional medical care is necessary following hairspray eye exposure requires careful assessment of symptoms, exposure circumstances, and response to initial treatment. The threshold for seeking medical attention should remain relatively low, given the potential for delayed complications and the difficulty in accurately assessing injury severity without specialised equipment. Emergency response protocols vary depending on the healthcare system and available resources, but certain presentations consistently require immediate professional intervention.
Ophthalmologist consultation criteria for aerosol eye injuries
Ophthalmological consultation becomes necessary when specific clinical indicators suggest potential serious injury or when initial treatment fails to provide expected improvement. Vision changes of any type, including decreased acuity, visual field defects, or persistent visual disturbances, warrant immediate specialist evaluation. Corneal involvement, indicated by cloudiness, visible epithelial defects, or fluorescein staining patterns, requires assessment by an eye care professional within 24 hours of exposure. Persistent severe pain that fails to respond to irrigation and basic comfort measures may indicate ongoing chemical injury requiring specialised treatment.
High-pressure exposures, particularly those occurring at close range (less than 30 centimetres), carry increased risk of mechanical injury and require ophthalmological assessment regardless of initial symptom severity. Individuals with pre-existing eye conditions, such as dry eye syndrome, previous corneal injuries, or those wearing contact lenses at the time of exposure, face higher complication risks and benefit from professional evaluation. Any exposure involving loss of consciousness or systemic symptoms requires immediate emergency medical care, as these may indicate significant inhalation exposure or systemic toxicity.
Accident and emergency department referral guidelines
Emergency department presentation is indicated for several specific circumstances following hairspray eye exposure. Immediate referral is necessary when irrigation facilities are inadequate for proper treatment, when multiple chemical exposures have occurred simultaneously, or when the exposed individual cannot cooperate with home treatment protocols. Paediatric exposures often require hospital assessment due to cooperation difficulties and the increased risk of serious injury in smaller eyes with proportionally larger exposure areas.
Systemic symptoms such as difficulty breathing, dizziness, nausea, or altered mental status indicate potential inhalation exposure or absorption of toxic compounds requiring comprehensive emergency evaluation. Failure to achieve symptom improvement after 30 minutes of appropriate irrigation warrants emergency department assessment, as this may indicate severe chemical injury or retained foreign material requiring surgical intervention. Any suspicion of intentional exposure, whether accidental overdose or deliberate self-harm, requires emergency psychiatric and medical evaluation.
Corneal abrasion documentation and treatment pathways
Corneal abrasions frequently accompany hairspray eye exposures, particularly when high-pressure discharge occurs at close range. Proper documentation requires fluorescein staining and slit-lamp examination to accurately assess the extent and depth of epithelial damage. Treatment protocols vary based on abrasion size, depth, and associated chemical injury, but typically include antibiotic prophylaxis, pain management, and close follow-up care. Large or central corneal abrasions may require pressure patching or therapeutic contact lens placement to promote healing and reduce discomfort.
The healing timeline for chemical-induced corneal abrasions often exceeds that of mechanical injuries due to ongoing inflammatory processes and potential persistent chemical effects. Follow-up examinations are typically scheduled at 24-48 hour intervals until epithelial healing is complete, with additional monitoring for delayed complications such as recurrent erosions or corneal scarring. Patient education regarding signs of complications and appropriate follow-up care is essential for optimal outcomes and prevention of long-term visual consequences.
Chemical burn classification using hughes classification system
The Hughes Classification System provides standardised grading for chemical ocular injuries, facilitating treatment planning and prognostic assessment. Grade I injuries involve only conjunctival irritation with intact corneal epithelium and carry excellent prognoses with minimal treatment. Grade II injuries include corneal epithelial defects with clear underlying stroma, typically healing within 1-3 weeks with appropriate care. Grade III injuries involve stromal involvement with corneal cloudiness and may result in permanent visual impairment despite aggressive treatment.
Grade IV injuries represent the most severe category, with extensive corneal and conjunctival damage, potential limbal stem cell destruction, and poor visual prognoses. Hairspray exposures rarely cause Grade IV injuries unless extremely high concentrations or prolonged contact occurs. However, the classification system helps guide treatment intensity and provides realistic expectations for patients and families regarding recovery timelines and potential outcomes.
Prevention strategies and aerosol application safety measures
Preventing hairspray-related eye injuries requires understanding common exposure scenarios and implementing appropriate safety measures during product use. Statistical analysis reveals that most accidental exposures occur during routine styling activities, with improper application techniques and environmental factors contributing significantly to injury risk. Professional hairstylists experience higher exposure rates due to occupational usage patterns, but residential users account for the majority of reported injuries. Understanding these patterns helps develop targeted prevention strategies for different user populations.
Proper application technique involves maintaining appropriate distance between the aerosol nozzle and the target area, typically 15-30 centimetres depending on the specific product and desired styling effect. Directional awareness is crucial, as wind currents, ventilation systems, and reflected spray patterns can redirect hairspray toward unprotected eyes. Environmental considerations include adequate ventilation to prevent aerosol accumulation and avoiding use in confined spaces where product concentrations may reach problematic levels.
Safety equipment considerations extend beyond basic eye protection to include proper storage practices that prevent accidental discharge and child access. Aerosol cans should be stored upright in cool, dry locations away from heat sources and direct sunlight. Regular inspection of nozzle mechanisms and actuator systems can identify potential malfunction risks that might cause unexpected discharge patterns or spray directions. User education regarding proper disposal of expired or damaged products prevents continued use of potentially hazardous containers that may malfunction during operation.
Professional environments require additional safety protocols, including adequate ventilation systems, personal protective equipment for high-exposure activities, and established emergency response procedures. Training programmes for salon staff should include recognition of chemical exposure symptoms, basic first aid techniques, and appropriate referral protocols for serious injuries. Regular safety audits and incident reporting systems help identify trends and implement targeted improvements in workplace safety practices.