Temple swelling during mastication presents a complex diagnostic challenge that requires careful evaluation of multiple anatomical systems. This condition affects thousands of individuals who experience uncomfortable enlargement or pressure in the temporal region whilst eating, speaking, or performing other jaw movements. The temporal area houses intricate networks of muscles, blood vessels, glandular structures, and neural pathways, all of which can contribute to swelling phenomena during masticatory activities.
Understanding the underlying mechanisms behind temple swelling during chewing requires an appreciation of the interconnected nature of orofacial structures. The symptoms may arise from temporomandibular dysfunction , salivary gland disorders, vascular complications, or infectious processes. Each potential cause presents distinct clinical patterns that healthcare professionals must recognise to provide appropriate treatment interventions.
Temporomandibular joint dysfunction and masticatory muscle inflammation
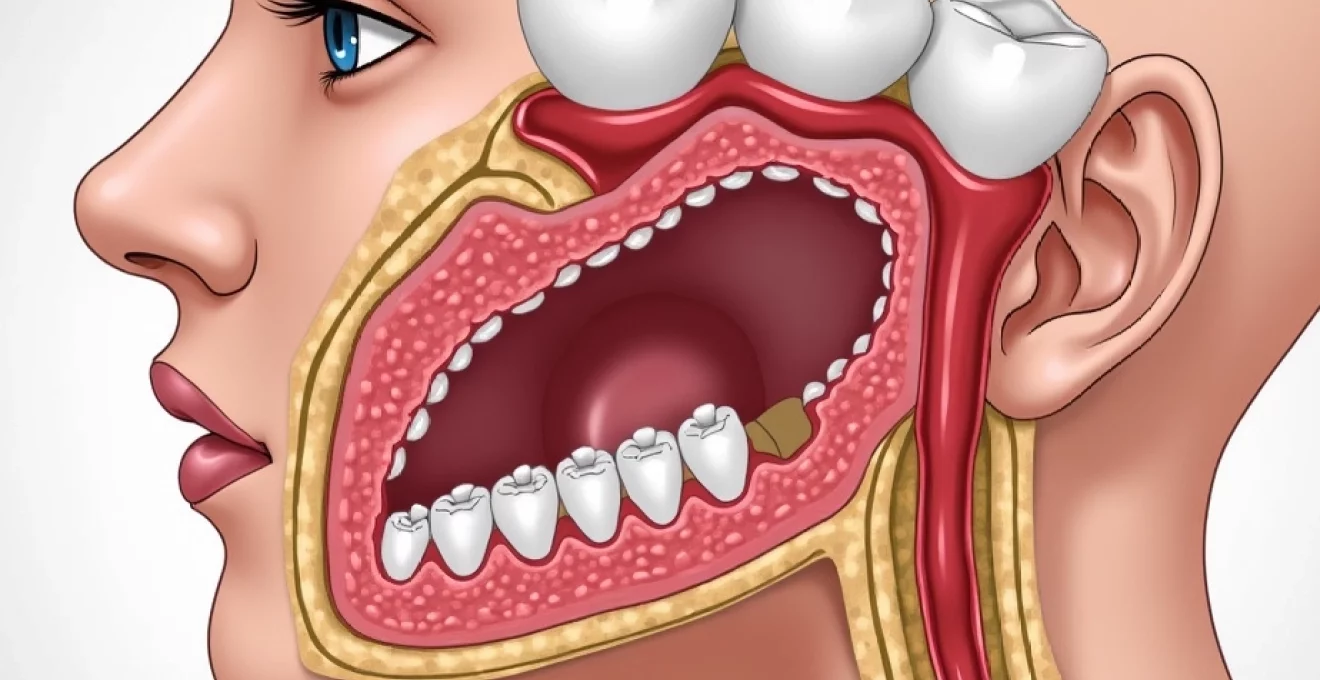
The temporomandibular joint represents one of the most complex articulations in the human body, facilitating essential functions including mastication, speech, and facial expression. When this intricate system experiences dysfunction, patients frequently develop temple swelling alongside other debilitating symptoms. The relationship between TMJ disorders and temporal region swelling stems from the intimate anatomical connections between joint structures and surrounding musculature.
Temporomandibular disorders encompass a broad spectrum of conditions affecting the joint complex, surrounding muscles, and associated neural pathways. These disorders frequently manifest as temple tenderness , facial asymmetry, and localised swelling that becomes more pronounced during masticatory activities. The inflammation process often extends beyond the joint capsule itself, involving neighbouring soft tissues and creating the characteristic swelling patterns observed in affected individuals.
Internal derangement of the TMJ disc complex during mastication
Internal derangement represents a significant contributor to temple swelling during chewing activities. The articular disc within the temporomandibular joint serves as a crucial shock absorber, facilitating smooth jaw movement whilst distributing mechanical forces across joint surfaces. When this disc becomes displaced or damaged, compensatory mechanisms activate throughout the masticatory system, often resulting in inflammation and swelling of surrounding tissues.
Disc displacement frequently occurs in anterior or anteromedial directions, creating mechanical interference during jaw opening and closing cycles. This disruption triggers inflammatory cascades within joint structures, leading to synovial fluid accumulation and capsular distension. The resulting swelling often extends beyond the immediate joint area, affecting temporal regions through fascial connections and shared vascular networks.
Medial and lateral pterygoid muscle spasm manifestations
The pterygoid muscles play fundamental roles in jaw positioning and masticatory function, with dysfunction in these structures contributing significantly to temple swelling patterns. The lateral pterygoid muscle, in particular, maintains intimate relationships with the TMJ disc complex, and spasm or hyperactivity in this muscle can directly influence joint mechanics and surrounding tissue inflammation.
Medial pterygoid muscle involvement often presents as deep-seated aching sensations that radiate towards temporal regions. When these muscles experience prolonged contraction or spasm, surrounding fascial planes become congested with inflammatory mediators, creating localised swelling that patients notice during chewing activities. The interconnected nature of masticatory muscle groups means that dysfunction in one area frequently propagates to adjacent structures.
Masseter muscle hypertrophy and compensatory mechanisms
Masseter muscle hypertrophy represents another important consideration in temple swelling evaluation. This powerful muscle of mastication can undergo adaptive changes in response to increased functional demands, parafunctional habits, or compensatory mechanisms following TMJ dysfunction. Hypertrophic changes often create visible and palpable swelling along the lateral facial contours.
Compensatory masseter hyperactivity frequently develops when other components of the masticatory system fail to function optimally. Patients with internal TMJ derangements often unconsciously modify their chewing patterns, placing excessive demands on the masseter muscles. This adaptation can lead to muscle enlargement, fascial tension, and associated swelling that becomes more pronounced during periods of increased masticatory activity.
Temporalis muscle fascial inflammation and trigger point development
The temporalis muscle directly overlies the temporal bone and represents a primary contributor to temple swelling during mastication. This fan-shaped muscle experiences significant mechanical stress during chewing activities, particularly in individuals with TMJ dysfunction or parafunctional habits. Fascial inflammation within the temporalis muscle complex creates localised swelling that patients readily identify.
Trigger point development within temporalis muscle fibres contributes to both pain and swelling patterns. These hyperirritable spots within muscle tissue generate referred pain patterns whilst simultaneously creating localised inflammatory responses. The resulting fascial tension and congestion manifests as temple swelling that intensifies during masticatory activities and may persist between meals.
Parotid gland pathology and ductal obstruction syndromes
The parotid glands represent the largest salivary glands in the human body, positioned directly adjacent to temporal regions and intimately connected to masticatory function. These serous glands produce substantial volumes of saliva during eating activities, and any disruption to normal glandular function can result in visible swelling that patients associate with chewing. Parotid pathology encompasses inflammatory conditions, obstructive disorders, and neoplastic processes that commonly present as temple area swelling.
Parotid gland swelling during mastication typically results from increased glandular activity combined with impaired drainage mechanisms. The glands naturally enlarge during salivary stimulation, but when drainage pathways become compromised, this physiological response becomes pathological. Understanding the various conditions affecting parotid function is essential for healthcare providers evaluating temple swelling complaints.
Stensen’s duct stenosis and sialolithiasis complications
Stensen’s duct serves as the primary drainage pathway for parotid gland secretions, opening into the oral cavity opposite the upper second molar. Stenosis or narrowing of this ductal system creates significant impedance to salivary flow, resulting in glandular distension and associated temple swelling. This condition becomes particularly problematic during eating when salivary production increases dramatically.
Sialolithiasis, or salivary stone formation, represents a common cause of ductal obstruction within the parotid system. These calcified deposits form within ductal lumens, creating partial or complete blockages that prevent normal salivary drainage. The resulting retrograde pressure causes glandular swelling that patients notice as temple enlargement during meals. Stone formation often occurs at ductal constriction points, with larger stones creating more significant obstructive symptoms.
Sjögren’s Syndrome-Related parotid swelling patterns
Sjögren’s syndrome represents an autoimmune condition that commonly affects salivary glands, including the parotid glands responsible for temple region contours. This chronic inflammatory disorder targets exocrine glands, leading to progressive destruction of glandular tissue and associated functional impairment. Patients with Sjögren’s syndrome frequently experience bilateral parotid swelling that becomes more pronounced during eating activities.
The autoimmune process in Sjögren’s syndrome creates characteristic inflammatory infiltrates within glandular tissue, disrupting normal secretory function whilst simultaneously causing glandular enlargement. This enlargement often presents as persistent temple fullness that intensifies during masticatory activities. The chronic nature of this condition distinguishes it from acute inflammatory processes and requires long-term management strategies.
Bacterial sialadenitis and purulent discharge mechanisms
Bacterial sialadenitis represents an acute inflammatory condition affecting parotid glands, commonly resulting from ascending infections through Stensen’s duct. These infections typically occur when salivary flow becomes compromised, allowing bacterial colonisation of ductal systems and subsequent glandular involvement. The resulting inflammatory response creates significant glandular swelling alongside systemic symptoms.
Purulent discharge mechanisms in bacterial sialadenitis involve the accumulation of inflammatory cells, bacterial toxins, and cellular debris within glandular structures. This purulent material creates pressure within the gland whilst simultaneously triggering intense inflammatory responses. Patients experience rapid onset temple swelling accompanied by pain, fever, and often purulent discharge from Stensen’s duct opening.
Warthin’s tumour and pleomorphic adenoma differential diagnosis
Parotid neoplasms represent important considerations in the evaluation of temple swelling, particularly when symptoms persist or progress over time. Warthin’s tumour, also known as papillary cystadenoma lymphomatosum, commonly affects parotid glands and presents as slowly enlarging masses within glandular tissue. These benign tumours often demonstrate characteristic bilateral occurrence and may become more noticeable during eating activities.
Pleomorphic adenoma represents the most common benign salivary gland tumour, frequently arising within parotid tissue and creating visible facial contour changes. These tumours typically present as firm, slowly growing masses that may contribute to temple region fullness. While generally asymptomatic, larger tumours can create mechanical effects that become more apparent during masticatory activities when surrounding tissues experience increased tension and movement.
Dental abscess formation and periapical pathology
Dental infections represent a frequently overlooked cause of temple swelling during chewing activities. Odontogenic infections can extend beyond immediate tooth structures, affecting surrounding soft tissues and creating fascial space involvement that manifests as temple region swelling. The anatomical pathways for infection spread from dental structures to temporal regions involve complex fascial planes and lymphatic drainage patterns.
Periapical abscesses developing from necrotic pulp tissue can create extensive inflammatory responses that extend far beyond the affected tooth. Upper molar infections, in particular, demonstrate propensity for superior and posterior spread due to anatomical relationships between tooth roots and surrounding bone structures. When these infections breach cortical bone boundaries, they can disseminate through fascial spaces, creating swelling patterns that affect temple regions.
The relationship between masticatory activities and dental abscess symptoms stems from mechanical pressure changes that occur during chewing. Biting forces create pressure variations within infected tissues, often exacerbating pain and swelling symptoms. Additionally, increased blood flow during mastication can intensify inflammatory responses, making temple swelling more noticeable during eating activities.
Chronic dental infections may present with more subtle swelling patterns compared to acute abscesses, but these conditions can still contribute to temple region fullness during chewing. Chronic periapical periodontitis creates persistent low-grade inflammation that can affect surrounding soft tissues. The resulting tissue congestion and lymphatic involvement may manifest as mild but persistent temple swelling that patients notice primarily during periods of increased masticatory activity.
Trigeminal neuralgia and atypical facial pain syndromes
Neurological conditions affecting the trigeminal nerve complex can contribute to temple region symptoms, including perceived swelling sensations during chewing activities. While these conditions primarily cause pain symptoms, associated inflammatory responses and muscle tension patterns can create actual tissue swelling alongside sensory disturbances. Understanding the relationship between trigeminal nerve pathology and temple swelling requires appreciation of both direct neural effects and secondary muscular responses.
Trigeminal neuralgia, characterised by severe episodic facial pain, can trigger protective muscle responses that contribute to tissue swelling. Patients experiencing acute neuralgic episodes often develop secondary muscle tension in masticatory muscles, leading to fascial congestion and localised swelling. The pain-muscle spasm-pain cycle creates perpetuating factors that maintain swelling responses even between acute episodes.
Atypical facial pain syndromes present with more complex symptom patterns that may include burning sensations, aching discomfort, and perceived swelling in affected distributions. These conditions often involve dysfunction of trigeminal nerve branches that innervate temporal regions, creating altered sensory processing that patients interpret as swelling. The relationship between neural dysfunction and actual tissue changes remains complex, with some patients demonstrating measurable swelling whilst others experience purely sensory phenomena.
Secondary muscle hyperactivity represents a common consequence of trigeminal nerve disorders, with affected individuals unconsciously altering masticatory patterns to avoid triggering painful episodes. These compensatory mechanisms often involve increased tension in temporalis and other masticatory muscles, creating mechanical conditions that favour tissue congestion and swelling. The resulting neuromuscular dysfunction perpetuates both pain and swelling symptoms, requiring comprehensive treatment approaches that address both neural and muscular components.
Lymphatic system involvement and cervical lymphadenopathy
The lymphatic drainage system plays a crucial role in maintaining tissue homeostasis throughout the head and neck region, with dysfunction in these networks contributing to swelling patterns that affect temple areas. Cervical lymphadenopathy can create drainage impedance that results in tissue congestion and associated swelling symptoms. Understanding lymphatic anatomy and pathology is essential for evaluating patients presenting with temple swelling during masticatory activities.
Regional lymph nodes receive drainage from multiple anatomical structures, including dental tissues, salivary glands, and masticatory muscles. When these nodes become enlarged or dysfunctional due to inflammatory or neoplastic processes, normal lymphatic drainage becomes compromised. The resulting tissue congestion can manifest as diffuse swelling that affects temple regions, particularly during periods of increased metabolic activity such as mastication.
Reactive lymphadenopathy commonly develops in response to odontogenic infections, upper respiratory tract infections, or other inflammatory conditions affecting the head and neck region. These enlarged lymph nodes create mechanical compression of lymphatic vessels whilst simultaneously reducing overall drainage capacity. Patients may notice temple swelling that intensifies during eating activities when tissue perfusion and lymphatic demands increase.
Systemic conditions affecting lymphatic function can also contribute to regional swelling patterns. Autoimmune disorders, certain medications, and metabolic conditions may impair lymphatic drainage capacity throughout the body, with head and neck regions being particularly susceptible to visible swelling changes. The temporal area, with its relatively thin soft tissue coverage, often demonstrates early signs of lymphatic congestion before other facial regions show similar changes.
Lymphatic dysfunction creates a cascading effect throughout interconnected drainage networks, with temple swelling often representing the visible manifestation of more widespread lymphatic congestion.
Diagnostic imaging protocols and clinical assessment techniques
Accurate diagnosis of temple swelling during chewing requires systematic evaluation combining clinical examination techniques with appropriate imaging modalities. The complexity of anatomical structures within the temporal region necessitates comprehensive assessment protocols that can differentiate between various potential causes. Healthcare providers must employ evidence-based diagnostic approaches to identify underlying pathology whilst avoiding unnecessary testing procedures.
Clinical examination begins with detailed history taking, focusing on symptom onset, duration, associated factors, and relationship to masticatory activities. Physical examination should include palpation of temporal regions, assessment of jaw movement patterns, evaluation of cranial nerve function, and inspection of intraoral structures. These initial assessments often provide crucial diagnostic information that guides subsequent imaging decisions.
Imaging protocols for temple swelling evaluation typically begin with conventional radiography to assess dental pathology and bony structures. Panoramic radiographs provide excellent visualisation of teeth, jaw bones, and TMJ structures, whilst intraoral radiographs offer detailed views of specific dental areas. These initial imaging studies can identify odontogenic causes of swelling whilst ruling out obvious skeletal abnormalities.
Advanced imaging modalities become necessary when initial assessments fail to identify clear causative factors. Magnetic resonance imaging provides superior soft tissue contrast, allowing detailed evaluation of TMJ disc position, masticatory muscle pathology, and salivary gland abnormalities. CT scanning offers excellent bony detail and can identify subtle fractures, joint space changes, or calcified deposits within salivary ducts.
The diagnostic process requires integration of clinical findings with imaging results to develop accurate diagnoses that guide appropriate treatment interventions.
Ultrasonography represents an increasingly valuable diagnostic tool for evaluating temple swelling, particularly when salivary gland pathology is suspected. This non-invasive modality provides real-time imaging of glandular structures, ductal systems, and surrounding soft tissues. Dynamic scanning during simulated chewing activities can reveal functional abnormalities that static imaging might miss.
Laboratory investigations may complement imaging studies in specific clinical scenarios. Complete blood counts can identify infectious or inflammatory processes, whilst specific autoimmune markers help diagnose conditions such as Sjögren’s syndrome. Bacterial culture of purulent discharge provides targeted antibiotic therapy guidance when infectious sialadenitis is suspected.
Specialised diagnostic techniques such as sialography can provide detailed evaluation of ductal systems when obstructive salivary gland disease is suspected. This contrast-enhanced imaging technique reveals ductal anatomy, identifies stenotic areas, and demonstrates the location of obstructive lesions. Modern sialographic techniques using MR or CT protocols offer improved patient comfort compared to conventional sialography whilst providing superior diagnostic information.
The integration of diagnostic findings requires careful correlation between clinical symptoms, physical
examination findings, imaging results, and laboratory data. This multidisciplinary approach ensures that underlying pathology is accurately identified whilst avoiding misdiagnosis that could lead to inappropriate treatment interventions. The temporal region’s complex anatomy requires systematic evaluation that considers all potential contributing factors.
Follow-up assessment protocols should be established for patients presenting with temple swelling during chewing, particularly when initial diagnostic evaluations fail to identify clear causative factors. Progressive symptoms or failure to respond to initial treatment interventions may necessitate additional imaging studies or specialist referrals. Early recognition of serious underlying conditions such as temporal arteritis or malignant processes requires vigilant clinical monitoring.
Differential diagnosis considerations must include both common and rare conditions that can present with similar symptom patterns. The systematic approach to diagnostic evaluation helps healthcare providers distinguish between benign functional disorders and serious pathological conditions requiring urgent intervention. Comprehensive documentation of diagnostic findings facilitates appropriate specialist referrals and ensures continuity of care across healthcare providers.
Patient education regarding diagnostic procedures helps reduce anxiety whilst improving compliance with recommended evaluations. Many patients experiencing temple swelling during chewing benefit from understanding the relationship between symptoms and underlying anatomical structures. This educational component enhances the therapeutic relationship whilst promoting active participation in the diagnostic process.
Effective diagnosis of temple swelling requires integration of clinical expertise with appropriate technology, ensuring that patients receive accurate diagnoses that lead to successful treatment outcomes.
The evolving landscape of diagnostic imaging continues to offer new opportunities for improved evaluation of temple swelling complaints. Artificial intelligence applications in medical imaging show promise for enhancing diagnostic accuracy whilst reducing interpretation time. These technological advances may ultimately improve patient outcomes by facilitating earlier detection of pathological conditions affecting the temporal region.
Cost-effectiveness considerations play an important role in diagnostic protocol development, with healthcare providers seeking to balance diagnostic accuracy with resource utilisation. Evidence-based guidelines help determine appropriate imaging sequences whilst avoiding unnecessary procedures that increase healthcare costs without improving patient outcomes. The judicious use of diagnostic resources ensures that healthcare systems can provide quality care whilst maintaining financial sustainability.
Quality assurance measures in diagnostic imaging ensure that patients receive accurate and reliable diagnostic information. Regular equipment calibration, radiologist training programmes, and peer review processes contribute to maintaining high standards of diagnostic accuracy. These quality initiatives directly impact patient care by reducing diagnostic errors and improving treatment planning precision.
The multidisciplinary nature of temple swelling evaluation often requires coordination between multiple healthcare specialties, including dentistry, oral and maxillofacial surgery, otolaryngology, and neurology. Effective communication between these specialties ensures comprehensive patient evaluation whilst avoiding duplicative testing procedures. This collaborative approach optimises diagnostic efficiency whilst providing patients with coordinated care that addresses all aspects of their condition.