The Harrington rod system revolutionised scoliosis surgery when it was introduced in the 1960s by Dr. Paul Harrington, establishing the foundation for modern spinal instrumentation techniques. This pioneering surgical approach transformed the treatment landscape for patients with severe spinal curvature, offering the first reliable method to internally straighten and stabilise the spine. For over two decades, the Harrington rod remained the gold standard for scoliosis correction, fundamentally changing how orthopaedic surgeons approached complex spinal deformities. Understanding how this system works provides crucial insight into both historical surgical evolution and the biomechanical principles that continue to influence contemporary spinal treatments.
Harrington rod system: surgical hardware components and biomechanical principles
The Harrington rod system represents a masterpiece of surgical engineering that addressed the complex three-dimensional nature of scoliotic deformity through ingenious mechanical principles. At its core, this system utilises distraction forces to gradually straighten the spine by applying tension along the concave side of the scoliotic curve. The fundamental concept relies on stretching the compressed tissues and vertebrae on the inside of the curve whilst simultaneously providing structural support during the fusion healing process.
Stainless steel rod construction and material properties
The Harrington rod itself consists of a straight stainless steel rod measuring approximately 6-10 millimetres in diameter, engineered with exceptional tensile strength to withstand the considerable forces generated within the human spine. The rod incorporates a sophisticated ratcheting mechanism that allows surgeons to apply controlled distraction forces incrementally during the procedure. This ratcheting system functions similarly to a car jack, enabling precise adjustments whilst maintaining the achieved correction throughout the surgical process.
Stainless steel was specifically chosen for its biocompatibility, corrosion resistance, and optimal strength-to-weight ratio. The material properties ensure that the rod can withstand decades of mechanical stress from daily activities whilst maintaining its structural integrity. The smooth surface finish minimises tissue irritation and reduces the risk of inflammatory responses that could compromise the surgical outcome.
Hook and clamp fixation mechanisms
The Harrington system achieves spinal fixation through strategically placed hooks that grip specific anatomical structures along the vertebral column. These hooks are positioned at the superior and inferior ends of the planned fusion, typically engaging the laminae or transverse processes of the vertebrae. The hook design incorporates multiple contact points to distribute forces evenly and prevent point loading that could cause bone failure or hardware loosening.
The clamp mechanisms within the hooks provide secure purchase on the bony anatomy whilst allowing for controlled movement during the distraction process. This dual functionality enables surgeons to maintain stable fixation whilst applying corrective forces, ensuring that the hardware remains securely attached throughout the procedure and subsequent healing period.
Posterior spinal fusion integration with harrington instrumentation
The Harrington rod serves as both a corrective device and a temporary internal scaffold during the spinal fusion process. Posterior spinal fusion involves decorticating the laminae, facet joints, and transverse processes to create bleeding bone surfaces that will ultimately grow together into a solid fusion mass. The rod maintains the corrected spinal alignment whilst this biological fusion occurs, typically requiring six to twelve months for complete consolidation.
Bone graft material, traditionally harvested from the patient’s iliac crest, is carefully placed along the prepared fusion bed. The Harrington rod prevents loss of correction during the vulnerable healing period when the bone graft is initially weak and unable to resist deforming forces. This integration of mechanical correction and biological healing represents the fundamental principle underlying all modern spinal fusion procedures.
Distraction and compression force distribution along the vertebral column
The biomechanical effectiveness of the Harrington system relies on its ability to apply sustained distraction forces along the concave aspect of the scoliotic curve. These forces gradually stretch the contracted soft tissues, including ligaments, muscles, and joint capsules, whilst simultaneously decompressing the vertebral bodies on the concave side. The distraction force typically ranges from 20-40 pounds, carefully calibrated to achieve correction without compromising spinal cord function.
Force distribution occurs primarily through the hook-bone interface, creating stress concentrations at the points of fixation. This concentration of forces, whilst effective for correction, also represents a potential weakness of the system, as high local stresses can lead to bone failure or hardware migration over time. The relatively limited points of fixation compared to modern systems means that intermediate vertebrae rely primarily on the fusion mass for long-term stability.
Patient selection criteria and pre-operative assessment for harrington rod insertion
Appropriate patient selection remains crucial for achieving optimal outcomes with Harrington rod instrumentation, requiring comprehensive evaluation of multiple factors that influence surgical success and long-term function. The assessment process involves detailed analysis of curve characteristics, skeletal maturity, overall health status, and patient expectations. Understanding these selection criteria helps determine whether the Harrington system represents the most appropriate treatment option for individual patients.
Cobb angle measurements and curve pattern analysis
The Cobb angle measurement serves as the primary radiographic parameter for determining surgical candidacy, with most Harrington rod procedures reserved for curves exceeding 45-50 degrees. This threshold reflects the balance between surgical risk and the natural history of scoliotic progression, as curves beyond this magnitude demonstrate significant likelihood of continued worsening even after skeletal maturity. Precise measurement technique ensures accurate assessment, utilising the most tilted vertebrae at the upper and lower ends of the curve.
Curve pattern analysis extends beyond simple angle measurement to include evaluation of curve flexibility, rotational component, and compensatory mechanisms throughout the spine. Flexibility assessment through side-bending radiographs helps predict the degree of correction achievable with distraction forces. Rigid curves may require additional procedures or alternative surgical approaches to achieve satisfactory results.
Skeletal maturity evaluation using risser sign grading
Skeletal maturity assessment plays a pivotal role in surgical timing, as the Harrington system can interfere with continued spinal growth in immature patients. The Risser sign provides a reliable indicator of skeletal maturity by evaluating ossification of the iliac crest apophysis. Patients with incomplete skeletal maturity face increased risks of complications, including the “crankshaft phenomenon” where continued anterior spinal growth can worsen deformity despite posterior fusion.
Additional maturity indicators include closure of the triradiate cartilage, vertebral body ring apophyses, and overall bone density assessment. These parameters help surgeons determine the optimal timing for intervention, balancing the need for correction against the potential for growth-related complications.
Thoracic kyphosis and lumbar lordosis balance assessment
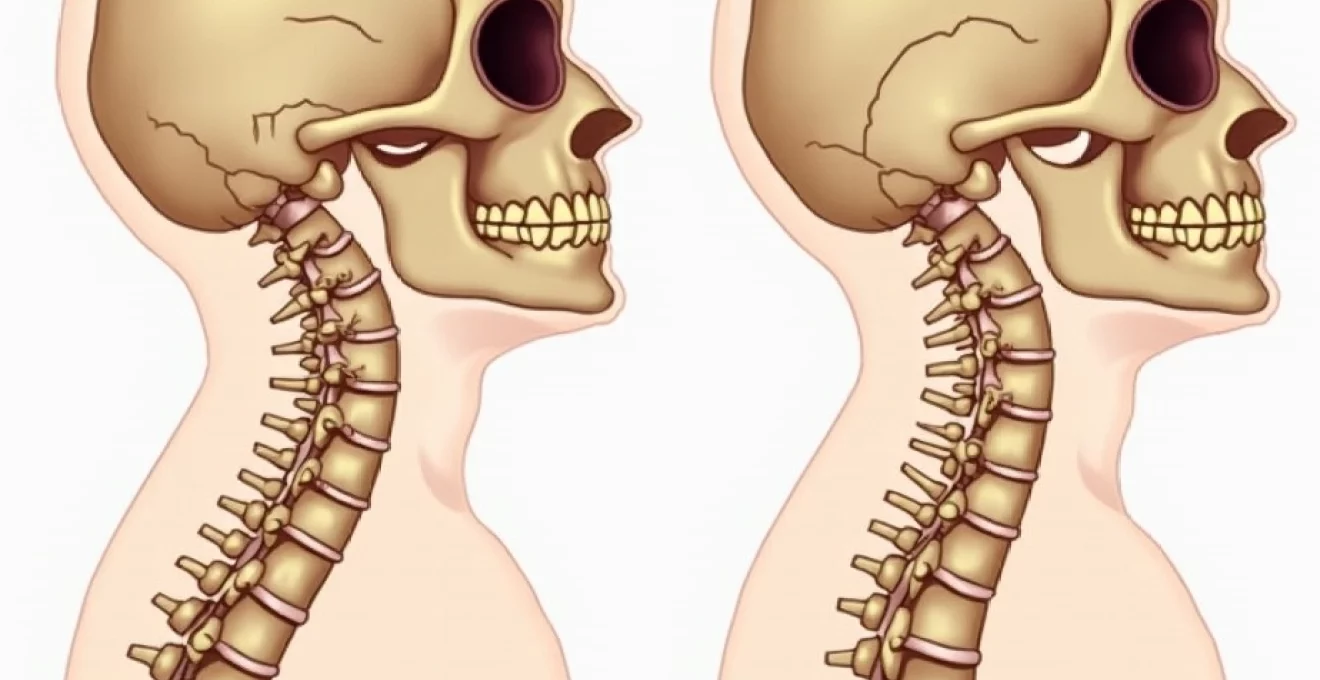
Sagittal plane alignment evaluation represents a critical component of pre-operative assessment, as the Harrington system historically demonstrated limited ability to restore normal spinal curvatures. The distraction forces tend to flatten the spine in the sagittal plane, potentially leading to “flat back syndrome” if proper attention is not paid to maintaining physiological lordosis and kyphosis. Detailed sagittal plane measurements help predict post-operative alignment and guide surgical planning.
The restoration of normal sagittal alignment remains one of the most challenging aspects of scoliosis surgery, requiring careful balance between coronal plane correction and maintenance of physiological spinal curvatures.
Pre-operative flexibility assessment in the sagittal plane helps determine the likelihood of maintaining acceptable sagittal alignment following Harrington rod insertion. Patients with pre-existing sagittal imbalance may be better candidates for alternative surgical approaches that provide superior three-dimensional correction capabilities.
Pulmonary function testing and respiratory capacity considerations
Severe thoracic scoliosis can significantly compromise pulmonary function through mechanical restriction of chest wall expansion and lung compression. Pre-operative pulmonary function testing provides baseline measurements and helps identify patients at risk for post-operative respiratory complications. Forced vital capacity (FVC) and forced expiratory volume (FEV1) serve as primary indicators of respiratory compromise.
Patients with severe restrictive lung disease may require multidisciplinary management including pulmonology consultation and potential pre-operative respiratory optimisation. The relationship between spinal deformity and pulmonary function influences both surgical timing and technique selection, as correction of thoracic curves can potentially improve respiratory capacity in some patients.
Harrington rod surgical technique: posterior spinal instrumentation procedure
The surgical technique for Harrington rod insertion follows a systematic approach that emphasises precise anatomical exposure, careful hardware placement, and meticulous attention to fusion preparation. This procedure typically requires 3-6 hours depending on curve complexity and represents a major surgical undertaking requiring specialised orthopaedic expertise. Understanding the technical aspects helps appreciate both the sophistication of the procedure and the potential complications that can arise.
Subperiosteal dissection and exposure of posterior elements
The surgical approach begins with a midline posterior incision extending from the upper instrumented vertebra to the lower instrumented level, typically spanning 8-12 vertebral segments. Careful subperiosteal dissection preserves the periosteal blood supply whilst providing adequate exposure of the laminae, facet joints, and transverse processes. This meticulous technique minimises bleeding and preserves the biological environment necessary for successful fusion.
Anatomical landmarks guide the dissection process, with particular attention paid to identifying the correct vertebral levels through palpation of specific structures. The exposure must be sufficiently wide to allow placement of bone graft material whilst avoiding excessive soft tissue stripping that could compromise healing. Electrocautery provides haemostasis whilst minimising thermal damage to surrounding tissues.
Facet joint preparation and decorticaton for arthrodesis
Preparation of the fusion bed involves systematic decortication of all bony surfaces that will be included in the fusion mass. The facet joints require complete removal of cartilage and exposure of bleeding subchondral bone to promote biological fusion. This process eliminates the natural joint spaces and creates an environment conducive to bone formation and eventual solid arthrodesis.
Decortication extends to the laminae and transverse processes, creating a roughened surface with multiple bleeding bone edges. The quality of fusion bed preparation directly correlates with fusion success rates, making this step critical to long-term outcomes. Bone wax should be used sparingly to maintain the biological activity of the prepared surfaces.
Hook placement at T4-L2 vertebral levels
Hook placement requires precise positioning at predetermined vertebral levels based on pre-operative planning and intraoperative fluoroscopic guidance. The superior hook typically engages the lamina or facet joint at the upper end of the curve, whilst the inferior hook secures to similar structures at the lower end. Proper hook orientation ensures optimal force transmission and minimises the risk of hardware failure or bone fracture.
The hook design incorporates specific anatomical contours that match the natural bone geometry, providing secure fixation without excessive stress concentration. Careful attention to hook positioning prevents impingement on neural structures whilst ensuring adequate bone purchase for long-term stability. Trial reduction helps confirm proper positioning before final rod insertion.
Rod contouring and progressive distraction application
The Harrington rod requires careful contouring to match the desired post-operative spinal alignment whilst accommodating the natural sagittal plane curvatures. This process involves gradual bending of the rod using specialised instruments, creating gentle curves that will maintain acceptable sagittal balance following correction. Over-aggressive contouring can lead to rod failure or inadequate correction.
Progressive distraction application utilises the ratcheting mechanism to gradually apply corrective forces over several minutes, allowing the spine to accommodate the changing forces. This gradual approach minimises the risk of neurological injury whilst achieving optimal correction. Continuous neurological monitoring ensures patient safety throughout the distraction process.
Iliac crest bone graft harvesting and posterior fusion mass creation
Autologous bone graft harvesting from the posterior iliac crest provides the biological foundation for successful spinal fusion. The harvesting technique involves careful dissection to avoid penetration of the inner cortex and potential injury to intra-pelvic structures. Adequate graft volume ensures sufficient biological material to bridge the entire fusion construct.
The harvested bone graft is carefully placed along the prepared fusion bed, creating continuous contact between graft material and decorticated bone surfaces. Proper graft placement ensures uniform distribution and optimal conditions for bone healing. The fusion mass should extend laterally to the tips of the transverse processes and provide continuous bridging between adjacent vertebral levels.
Comparison with modern spinal instrumentation: Cotrel-Dubousset and pedicle screw systems
The evolution from Harrington rod instrumentation to modern spinal systems represents a quantum leap in surgical sophistication and patient outcomes. Contemporary systems like the Cotrel-Dubousset (CD) instrumentation and pedicle screw constructs address many of the fundamental limitations inherent in the original Harrington design. These advances include improved three-dimensional correction capabilities, enhanced fixation strength, and superior restoration of normal spinal alignment.
Modern multiple hook and rod systems utilise bilateral rods connected by cross-linking devices, providing significantly greater torsional stability compared to the single-rod Harrington system. The CD system, introduced in 1984, pioneered the use of multiple hooks at various vertebral levels, allowing surgeons to apply different force vectors simultaneously. This multi-point fixation distributes loads more evenly and reduces stress concentrations that could lead to hardware failure or bone fracture.
Pedicle screw systems represent the current gold standard for spinal instrumentation, offering unparalleled fixation strength and three-column vertebral control. Unlike the Harrington system, which relies solely on posterior element fixation, pedicle screws engage the strongest portion of the vertebra and provide rigid three-dimensional control. This enhanced fixation allows for more aggressive correction manoeuvres whilst reducing the risk of hardware loosening or failure.
The transition from single-rod distraction systems to modern multi-rod constructs with segmental fixation has fundamentally transformed the biomechanical principles underlying spinal deformity correction.
The ability to contour rods in multiple planes represents another significant advancement over the Harrington system. Modern rods can be shaped to restore physiological sagittal alignment whilst maintaining coronal plane correction, addressing one of the primary weaknesses of distraction-based systems. This three-dimensional correction capability has dramatically reduced the incidence of flat back syndrome and improved long-term functional outcomes.
Segmental fixation with modern systems eliminates many of the complications associated with limited fixation points in the Harrington construct. Multiple attachment points distribute forces more evenly and provide redundancy in case of individual fixation failure. This enhanced stability often eliminates the need for post-operative bracing, improving patient comfort and facilitating earlier mobilisation.
Long-term outcomes and harrington Rod-Related complications
Long-term follow-up studies of patients with Harrington rod instrumentation reveal a complex picture of outcomes that must balance the historical context of available alternatives against modern expectations for spinal surgery. Whilst the Harrington system successfully prevented progression in most patients and achieved meaningful correction of major curves, several characteristic complications have emerged over decades of follow-up. Understanding these outcomes provides valuable insight into the evolution of scoliosis surgery and informs contemporary treatment decisions.
Flat back syndrome represents the most significant long-term complication associated with Harrington rod instrumentation, affecting approximately 20-40% of patients depending on the extent of lumbar involvement. This condition results from loss of normal lumbar lordosis due to the distraction forces applied during correction. Patients develop a characteristic forward-leaning posture, difficulty standing upright, and progressive fatigue with prolonged standing or walking. The biomechanical alterations place excessive stress on adjacent spinal segments and can lead to accelerated degenerative changes.
Pseudoarthrosis, or failure of solid fusion to occur, presents another significant concern with reported rates ranging from 5-15% in Harrington rod patients. The limited fixation points and relatively high stress concentrations increase the risk of fusion failure compared to modern segmental fixation systems. Pseudoarthrosis typically manifests as persistent pain, progressive loss of correction, and eventual hardware failure. Revision surgery is often necessary to achieve solid fusion and address associated complications.
Hardware-related complications include rod fracture, hook dislodgement, and implant migration, occurring in approximately 5-10% of patients over extended follow-up periods. The fatigue properties of stainless steel, whilst excellent, are not infinite, and rod fractures can occur after decades of cyclical loading. Hook-related complications often result from inadequate initial fixation or progressive bone remodelling around the implants.
Adjacent segment degeneration affects a substantial proportion of long-term Harrington rod patients, particularly those with
extensions to the lower lumbar spine. The immobilisation of multiple spinal segments places increased mechanical demands on the unfused vertebrae above and below the construct, accelerating wear patterns and potentially requiring future surgical intervention. Studies indicate that up to 30% of patients may develop clinically significant adjacent segment problems within 20 years of surgery.
Pain outcomes following Harrington rod surgery demonstrate considerable variability, with most patients experiencing significant improvement in the first several years post-operatively. However, long-term pain patterns often differ from initial expectations, with some patients developing new types of discomfort related to loss of spinal flexibility or hardware-related issues. The inability to bend and twist naturally affects daily activities and may limit participation in certain recreational pursuits.
Respiratory function outcomes generally show modest improvements in patients with severe pre-operative restrictive patterns, though the gains are often less dramatic than initially hoped. The correction of thoracic curves can provide some expansion of chest cavity volume, but the loss of spinal flexibility may partially offset these benefits. Long-term respiratory health requires ongoing monitoring, particularly in patients with residual restrictive patterns.
Revision surgery rates for Harrington rod patients range from 10-25% over extended follow-up periods, with most revisions addressing flat back syndrome, pseudoarthrosis, or hardware-related complications. These revision procedures are typically more complex than the original surgery due to scar tissue formation, altered anatomy, and the need to work around existing hardware. Modern revision techniques often involve conversion to contemporary instrumentation systems with improved biomechanical properties.
The legacy of Harrington rod instrumentation serves as both a testament to surgical innovation and a reminder that even successful treatments may require modification as our understanding of spinal biomechanics evolves.
Patient satisfaction surveys reveal a complex relationship between objective surgical outcomes and subjective patient experience. Whilst most patients express gratitude for the prevention of further curve progression and the cosmetic improvements achieved, many also report limitations that were not fully appreciated at the time of surgery. This highlights the importance of comprehensive pre-operative counselling regarding long-term expectations and potential complications.
Post-operative management and rehabilitation protocols following harrington rod surgery
The post-operative management following Harrington rod insertion requires a carefully orchestrated approach that balances the need for adequate immobilisation with the goal of maintaining overall patient health and function. The immediate post-surgical period presents unique challenges related to pain management, neurological monitoring, and gradual mobilisation whilst protecting the surgical construct during the critical healing phase. Understanding these protocols helps ensure optimal outcomes and minimises the risk of complications that could compromise long-term success.
Immediate post-operative care focuses on neurological monitoring and pain management during the first 24-48 hours following surgery. Continuous assessment of motor and sensory function helps identify any potential spinal cord or nerve root complications that might require immediate intervention. The wake-up test, performed during surgery, provides initial confirmation of neurological integrity, but ongoing vigilance remains essential throughout the early recovery period. Pain management typically involves a multimodal approach combining narcotic medications with anti-inflammatory agents and muscle relaxants.
The bracing protocol represents a critical component of post-operative management, as the Harrington rod’s limited fixation points require external support to maintain correction during the fusion healing process. Most patients require a custom-fabricated thoracolumbosacral orthosis (TLSO) that must be worn continuously for the first 3-6 months following surgery. The brace design must accommodate the post-operative anatomy whilst providing adequate support to prevent loss of correction or hardware failure.
Gradual mobilisation begins within the first few days post-operatively, following a structured progression that respects the healing tissues whilst preventing the complications associated with prolonged bed rest. Initial activities focus on basic self-care and short-distance ambulation with appropriate support. The progression of activities must be carefully monitored to ensure that increased demands do not compromise the surgical construct or cause excessive discomfort.
Physical therapy plays a crucial role in the rehabilitation process, though the approach differs significantly from that used with modern instrumentation systems. The emphasis remains on maintaining flexibility in unfused segments whilst respecting the limitations imposed by the rigid Harrington construct. Breathing exercises become particularly important for patients with thoracic fusions to maintain optimal pulmonary function and prevent respiratory complications.
Return to normal activities follows a structured timeline that typically extends over 6-12 months, depending on individual healing rates and the extent of the surgical procedure. Academic activities can usually resume within 2-4 weeks, whilst more demanding physical activities may require 6-12 months before full participation is safe. Contact sports and high-impact activities often remain permanently restricted due to the risk of hardware failure or adjacent segment injury.
Long-term follow-up protocols include regular radiographic monitoring to assess fusion progression, hardware integrity, and overall spinal alignment. These evaluations typically occur at 3, 6, 12, and 24 months post-operatively, with annual assessments thereafter. The development of adjacent segment degeneration, loss of sagittal balance, or hardware-related complications requires ongoing surveillance throughout the patient’s lifetime.
Activity modification counselling helps patients understand the permanent limitations associated with spinal fusion whilst maximising their potential for productive, fulfilling lives. The loss of spinal flexibility affects many daily activities in subtle ways that may not be immediately apparent. Patients benefit from specific guidance regarding proper body mechanics, ergonomic considerations, and strategies for maintaining overall physical fitness within the constraints of their surgical construct.
The psychological aspects of recovery deserve particular attention, as the adjustment to life with a rigid spine can present unexpected challenges. Many patients experience a period of grief related to the loss of normal spinal function, despite their appreciation for the correction achieved. Support groups and counselling resources can provide valuable assistance during this adjustment period, helping patients develop realistic expectations and coping strategies for long-term success.