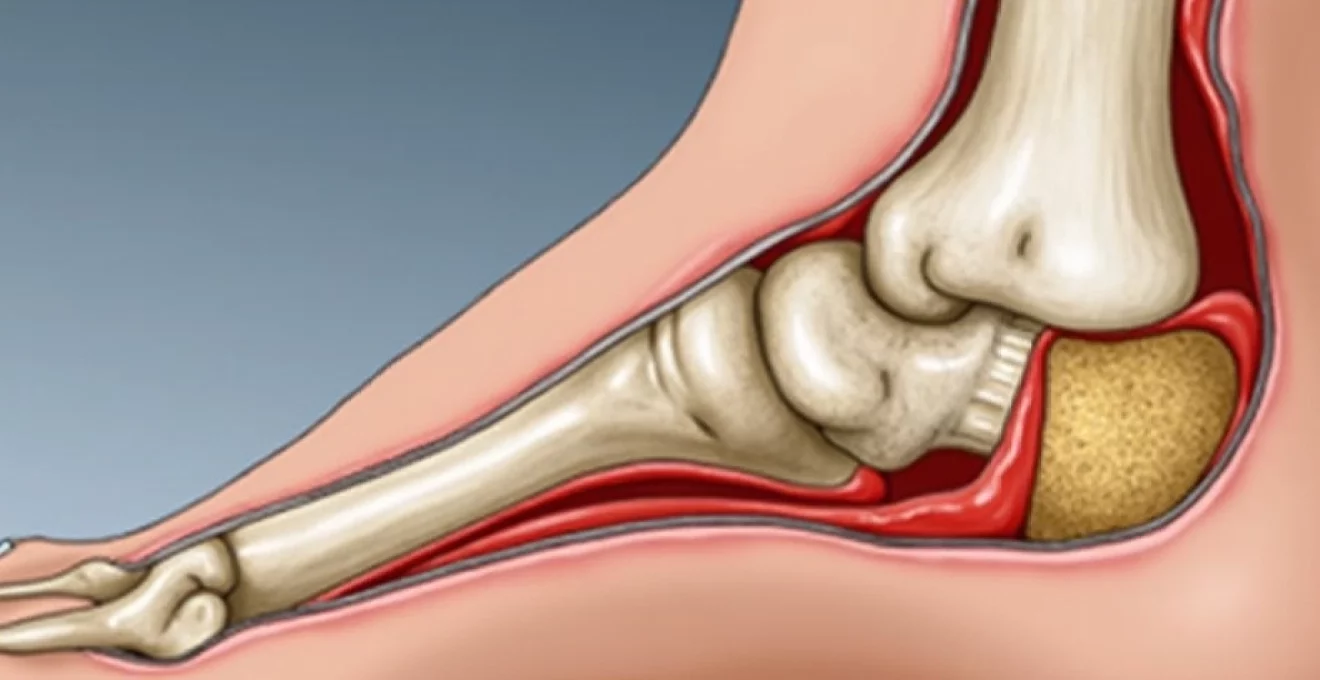
The journey through calcaneal osteotomy presents a complex landscape of surgical precision, recovery challenges, and long-term outcomes that significantly impact patient quality of life. This corrective procedure, designed to address various foot deformities including severe flatfoot conditions, represents one of the most transformative yet demanding surgical interventions in orthopaedic foot and ankle surgery. Understanding the intricacies of recovery, from initial post-operative challenges to eventual return to athletic activities, provides crucial insights for patients contemplating this life-changing procedure.
The surgical correction of calcaneal alignment disorders has evolved considerably over recent decades, with refined techniques offering improved outcomes for patients suffering from debilitating foot deformities. Modern calcaneal osteotomy techniques address not only the mechanical aspects of foot alignment but also the functional restoration necessary for patients to return to their desired activity levels, including high-impact sports and endurance activities like distance running.
Understanding calcaneal osteotomy: dwyer and evans surgical techniques
The foundation of successful calcaneal osteotomy lies in selecting the appropriate surgical technique based on individual patient pathology and desired correction outcomes. Contemporary orthopaedic surgeons employ various osteotomy methods, each designed to address specific deformity patterns and biomechanical abnormalities that contribute to patient symptoms and functional limitations.
The evolution of calcaneal correction techniques has produced sophisticated approaches that consider three-dimensional deformity patterns rather than simply addressing isolated sagittal or coronal plane abnormalities. Surgical planning precision has become increasingly important as surgeons recognise that successful outcomes depend heavily on accurate pre-operative assessment and meticulous intraoperative execution.
Lateral closing wedge osteotomy for cavus foot correction
The Dwyer lateral closing wedge osteotomy represents a time-tested approach for correcting hindfoot varus deformities commonly associated with cavus foot conditions. This technique involves removing a carefully calculated triangular bone wedge from the lateral aspect of the calcaneus, allowing for controlled correction of heel alignment and improved weight distribution across the foot.
Surgical success with lateral closing wedge techniques depends significantly on accurate wedge size calculation and precise osteotomy placement. The procedure typically addresses heel varus angles ranging from 10 to 25 degrees, with correction limited by soft tissue constraints and the need to maintain adequate bone contact for healing. Patient selection criteria for this technique include flexible deformities without significant arthritic changes in surrounding joints.
Medial opening wedge osteotomy applications in flatfoot deformity
Medial opening wedge calcaneal osteotomy has gained prominence in treating severe flatfoot deformities, particularly when combined with other reconstructive procedures. This technique involves creating a controlled fracture through the calcaneal tuberosity and inserting bone graft material to achieve desired correction angles while maintaining structural integrity.
The primary advantage of opening wedge techniques lies in their ability to achieve significant correction without bone loss, making them particularly valuable for patients requiring substantial realignment. However, the procedure demands careful attention to graft selection and fixation methods to ensure reliable healing and long-term stability. Healing timelines for opening wedge procedures often extend beyond those seen with closing wedge techniques due to the biological demands of graft incorporation.
Z-cut calcaneal lengthening osteotomy indications
The Z-cut or step-cut calcaneal lengthening osteotomy provides surgeons with the ability to address both length and angular deformities simultaneously. This sophisticated technique creates a controlled zigzag cut through the calcaneus, allowing for translation and rotation while maintaining bone contact surfaces for reliable healing.
Clinical applications for Z-cut techniques include complex flatfoot reconstructions where simple angular correction proves insufficient. The procedure’s versatility allows surgeons to address multiple deformity components through a single osteotomy site, potentially reducing overall surgical morbidity. Technical demands for this approach require considerable surgical expertise and careful pre-operative planning to achieve optimal outcomes.
Percutaneous calcaneal displacement osteotomy protocol
Minimally invasive percutaneous calcaneal displacement osteotomy represents the latest evolution in heel bone correction techniques. This approach utilises small incisions and specialised instrumentation to achieve controlled calcaneal repositioning while minimising soft tissue disruption and accelerating recovery timelines.
The percutaneous approach offers several advantages, including reduced surgical morbidity, decreased post-operative pain, and potentially faster return to activity. However, the technique requires extensive training and careful patient selection to ensure appropriate candidates receive this advanced treatment option. Long-term outcomes from percutaneous techniques continue to be evaluated as the procedure gains wider acceptance in the orthopaedic community.
Pre-operative assessment and surgical planning considerations
Comprehensive pre-operative evaluation forms the cornerstone of successful calcaneal osteotomy outcomes, requiring detailed analysis of patient symptoms, functional limitations, and underlying pathological processes. The assessment process extends far beyond simple radiographic measurements, encompassing dynamic foot function analysis, patient activity goals, and realistic outcome expectations.
Modern pre-operative planning incorporates advanced imaging technologies, biomechanical assessment tools, and sophisticated surgical planning software to optimise correction strategies. Patient counselling during this phase proves crucial for setting appropriate expectations regarding recovery timelines, activity restrictions, and potential complications that may arise during the healing process.
Weight-bearing radiographic analysis and böhler’s angle measurement
Weight-bearing radiographic assessment provides fundamental information about foot alignment and load distribution patterns that influence surgical planning decisions. Standard imaging protocols include anteroposterior, lateral, and oblique views of the foot and ankle, with additional specialised projections as clinically indicated.
Böhler’s angle measurement serves as a critical parameter for assessing calcaneal alignment and monitoring correction outcomes. Normal values typically range from 20 to 40 degrees, with significant deviations indicating pathological conditions requiring surgical intervention. Measurement accuracy depends on proper patient positioning and image quality, making standardised protocols essential for reliable assessment.
CT scan evaluation for Three-Dimensional deformity assessment
Computed tomography scanning has revolutionised pre-operative planning by providing detailed three-dimensional visualisation of bone architecture and deformity patterns. Weight-bearing CT technology, where available, offers unprecedented insight into foot mechanics under physiological loading conditions.
CT evaluation proves particularly valuable for complex deformity cases where traditional radiography provides insufficient detail for surgical planning. The technology allows surgeons to assess bone quality, identify potential complications, and plan optimal osteotomy placement with enhanced precision. Advanced imaging techniques have significantly improved surgical outcomes by enabling more accurate correction strategies.
Pedobarographic testing for plantar pressure distribution analysis
Pedobarographic analysis provides objective data about foot function and pressure distribution patterns that complement traditional imaging studies. This technology reveals how patients actually load their feet during walking, identifying areas of excessive pressure that contribute to symptoms and functional limitations.
Pre-operative pedobarographic testing establishes baseline measurements that can be compared with post-operative results to assess functional improvement. The data helps surgeons understand the relationship between structural deformity and functional impairment, guiding surgical decision-making and patient counselling. Functional assessment through pedobarography has become an increasingly important component of comprehensive foot and ankle evaluation.
Patient selection criteria and contraindications assessment
Appropriate patient selection represents perhaps the most critical factor determining calcaneal osteotomy success rates. Ideal candidates typically present with symptomatic deformities that have failed conservative management, realistic functional goals, and adequate bone quality for surgical correction.
Contraindications include active infection, severe peripheral vascular disease, uncontrolled diabetes with poor wound healing potential, and unrealistic patient expectations. Age alone rarely serves as an absolute contraindication, though overall health status and activity demands influence surgical recommendations. Risk stratification helps surgeons identify patients most likely to achieve successful outcomes while minimising potential complications.
Surgical procedure and intraoperative challenges
The technical execution of calcaneal osteotomy demands meticulous attention to anatomical relationships, precise bone cutting techniques, and careful soft tissue management. Surgical success depends heavily on the surgeon’s ability to navigate complex three-dimensional anatomy while achieving accurate correction and secure fixation.
Intraoperative challenges frequently arise due to the calcaneus’s dense bone structure, proximity to neurovascular structures, and the precision required for optimal alignment correction. Surgical expertise development requires extensive training and experience with various osteotomy techniques to handle unexpected complications and achieve consistent outcomes.
Lateral approach technique and sural nerve protection
The lateral surgical approach provides excellent visualisation of the calcaneal tuberosity while minimising disruption to important medial structures. Careful dissection through skin, subcutaneous tissue, and deep fascia layers allows surgeons to access the osteotomy site while protecting vital neurovascular structures.
Sural nerve protection represents a critical technical consideration during lateral approach procedures. The nerve’s variable anatomical course requires careful identification and gentle retraction to prevent injury that could result in permanent sensory deficit. Anatomical knowledge and surgical technique refinement help minimise nerve-related complications and improve patient satisfaction with outcomes.
Osteotomy site preparation and wedge calculation methods
Precise osteotomy site preparation involves careful marking of bone cutting lines, drill hole placement, and saw blade orientation to achieve desired correction angles. Wedge size calculation requires consideration of pre-operative measurements, desired correction amounts, and bone geometry factors that influence final alignment.
Mathematical calculations for wedge removal or opening must account for three-dimensional correction requirements and potential overcorrection to compensate for settling or loss of correction during healing. Precision planning tools, including computer-assisted navigation systems, have enhanced surgeons’ ability to achieve accurate corrections consistently.
Internal fixation using AO screws and plate systems
Secure internal fixation ensures proper healing and maintenance of correction throughout the recovery period. Modern fixation options include various screw configurations, low-profile plates, and combination systems designed specifically for calcaneal osteotomy applications.
Fixation selection depends on osteotomy type, bone quality, patient activity level, and surgeon preference. Compression screws provide excellent stability for closing wedge procedures, while plate systems offer superior control for complex corrections or compromised bone quality situations. Hardware selection significantly influences healing rates and long-term outcome success.
Intraoperative fluoroscopy guidance and alignment verification
Real-time fluoroscopic imaging allows surgeons to verify correction accuracy and fixation placement during the procedure. Multiple imaging planes provide comprehensive visualisation of bone alignment and hardware positioning to ensure optimal results.
Intraoperative imaging protocols include systematic evaluation of correction angles, screw placement, and overall foot alignment. Surgeons must be proficient in fluoroscopic interpretation to make real-time adjustments when necessary. Image guidance technology has become indispensable for achieving consistent surgical outcomes and minimising revision requirements.
Post-operative recovery timeline and rehabilitation protocol
The post-operative recovery journey following calcaneal osteotomy presents a carefully orchestrated progression through distinct phases, each with specific goals, limitations, and milestones. Understanding this timeline proves essential for patients to maintain realistic expectations and achieve optimal long-term outcomes. The initial weeks focus primarily on wound healing and bone union initiation, while later phases emphasise progressive weight-bearing and functional restoration.
Recovery complexity varies significantly based on osteotomy type, patient factors, and adherence to post-operative protocols. Early mobilisation strategies have evolved to balance healing requirements with the benefits of controlled movement, leading to improved outcomes and reduced complications compared to traditional immobilisation approaches.
The first six to eight weeks typically require strict non-weight-bearing status with cast or boot immobilisation to protect the osteotomy site during critical healing phases. Patients must navigate daily activities using assistive devices while managing post-operative pain and swelling. This period often presents the greatest challenges for active individuals accustomed to regular exercise and sports participation.
During the initial recovery phase, patients frequently experience frustration with mobility limitations and uncertainty about long-term outcomes. However, strict adherence to weight-bearing restrictions during this critical period significantly influences ultimate surgical success and return to desired activity levels.
Progressive weight-bearing typically begins between eight to twelve weeks post-operatively, based on radiographic evidence of bone healing and clinical assessment of surgical site stability. This transition requires careful monitoring and gradual activity advancement to prevent complications while encouraging functional improvement. Rehabilitation progression must be individualised based on healing rates, patient goals, and underlying health factors.
The six-month milestone represents a critical juncture where most patients experience significant functional improvement and reduced activity restrictions. However, complete healing and optimal outcomes often require the full twelve-month recovery period, particularly for patients seeking return to high-impact activities like running or competitive sports.
Managing complications: nonunion and hardware failure
Complication management represents a crucial aspect of calcaneal osteotomy care, with nonunion and hardware failure constituting the most significant challenges surgeons and patients face during recovery. These complications can substantially impact functional outcomes and may require additional surgical intervention to achieve desired results.
Nonunion rates for calcaneal osteotomy procedures typically range from 2% to 8%, depending on surgical technique, patient factors, and post-operative compliance. Risk factors include smoking, diabetes, poor nutritional status, and premature weight-bearing activities. Early recognition of nonunion signs allows for prompt intervention and improved salvage outcomes.
Hardware failure can manifest as screw breakage, plate fracture, or loss of fixation, often resulting from excessive loading or inadequate initial stability. Modern fixation systems have significantly reduced failure rates, but patient compliance with activity restrictions remains essential for preventing mechanical complications. Revision surgery may be necessary for symptomatic hardware failure or persistent nonunion situations.
Successful complication management requires early recognition, prompt intervention, and realistic patient counselling about potential impact on final outcomes. Most complications can be successfully managed with appropriate treatment, though recovery timelines may be extended.
Prevention strategies focus on optimising patient health before surgery, using appropriate fixation methods, and ensuring strict adherence to post-operative protocols. Smoking cessation, diabetes control, and nutritional optimisation significantly reduce complication risks and improve healing outcomes.
Long-term outcomes and functional assessment results
Long-term functional outcomes following calcaneal osteotomy demonstrate significant variability based on numerous factors including pre-operative deformity severity, surgical technique, patient compliance, and individual healing characteristics. Comprehensive outcome assessment requires evaluation of pain levels, functional capacity, radiographic alignment, and patient satisfaction measures extending well beyond the initial recovery period.
Recent studies indicate that approximately 80-85% of patients achieve good to excellent outcomes at two-year follow-up, with pain relief and functional improvement representing the primary success measures. However, return to high-impact activities such as distance running requires careful evaluation and may not be appropriate for all patients regardless of surgical success. Activity modification often becomes necessary even after successful correction to maintain long-term joint health and prevent degenerative changes.
Pain relief represents the most consistent and predictable outcome following successful calcaneal osteotomy, with most patients experiencing significant improvement in both rest and activity-related discomfort. However, complete pain elimination may not occur in all cases, particularly for patients with pre-existing arthritic changes or chronic soft tissue irritation. Realistic expectations regarding pain levels help patients appreciate the degree of improvement achieved through surgical intervention.
Functional capacity assessment reveals that most patients can return to moderate-impact activities including walking, swimming, and recreational cycling within six to twelve months post-operatively. Return to high-impact sports such as tennis or running requires individual evaluation and may be limited by factors beyond the osteotomy healing. Sport-specific rehabilitation programs can help optimise outcomes for athletically active patients.
The definition of surgical success varies significantly among patients, with some prioritising pain relief while others focus on return to specific activities. Comprehensive pre-operative counselling helps establish realistic goals and improves overall satisfaction with outcomes.
Radiographic alignment correction typically maintains well over time when adequate healing occurs and patients comply with activity modifications. However, some degree of correction loss may occur, particularly in patients who return to high-demand activities or have underlying
connective tissue disorders that predispose to continued deformity progression.
Patient satisfaction surveys consistently demonstrate high levels of contentment with surgical outcomes, particularly regarding pain relief and improved daily function. However, satisfaction levels may decrease among patients who had unrealistic expectations about return to previous activity levels or who experience complications during recovery. Pre-operative counselling quality significantly influences long-term satisfaction ratings and patient perception of surgical success.
The ability to return to running activities, specifically the 5-kilometer distance mentioned in patient forums, requires careful individual assessment and typically occurs in select patients with excellent healing, good pre-operative conditioning, and appropriate biomechanical factors. Studies suggest that approximately 60-70% of previously active runners can return to some level of jogging, though many require pace reduction or distance limitations to maintain comfort and prevent complications.
Long-term success in calcaneal osteotomy extends beyond the surgical technique itself, encompassing comprehensive patient education, realistic expectation setting, and ongoing support throughout the extended recovery process. The most satisfied patients are those who understand the procedure’s limitations while appreciating the significant functional improvements achieved.
Degenerative joint changes in adjacent foot and ankle joints represent a potential long-term concern, particularly for patients who return to high-impact activities. Regular monitoring and preventive strategies, including appropriate footwear and activity modification, help minimise the risk of secondary arthritic conditions that could compromise long-term outcomes.
The evolution of calcaneal osteotomy techniques continues to improve outcomes and reduce complications, with emerging technologies such as patient-specific instrumentation and advanced fixation systems showing promise for further enhancement of surgical results. Future developments in surgical technique and post-operative management protocols may further improve the prospects for patients seeking return to demanding athletic activities following corrective heel bone surgery.
For patients considering calcaneal osteotomy, the evidence suggests that while complete return to pre-injury activity levels may not always be possible, significant functional improvement and pain relief can be achieved in the majority of cases. The key lies in appropriate patient selection, meticulous surgical technique, and comprehensive post-operative management extending through the full twelve-month healing period and beyond.